November 2018
Long gone are the days when a health insurer would operate on a purely indemnity model, just processing and paying medical claims and then passing on the inevitable Medical Trend every year in the form of increased premiums. Annual double-digit Medical Trend increases are not financially sustainable for captives, which cannot easily pass on the increases to their local businesses.
“Today, health insurers and healthcare captives are far more engaged in the health (and health delivery) of their covered populations. They are more proactive. This is a shift from payer to partner,” says Eric Butler, Director, Global Health & Wellness at GEB.
“For healthcare captives the focus of this partnership is increasingly about addressing trends and cost drivers, which often means addressing changes in the burden of illness for a given population, or rather, trying to have a positive impact on the current and future health of all individuals insured.”
How is GEB ensuring this leading role?
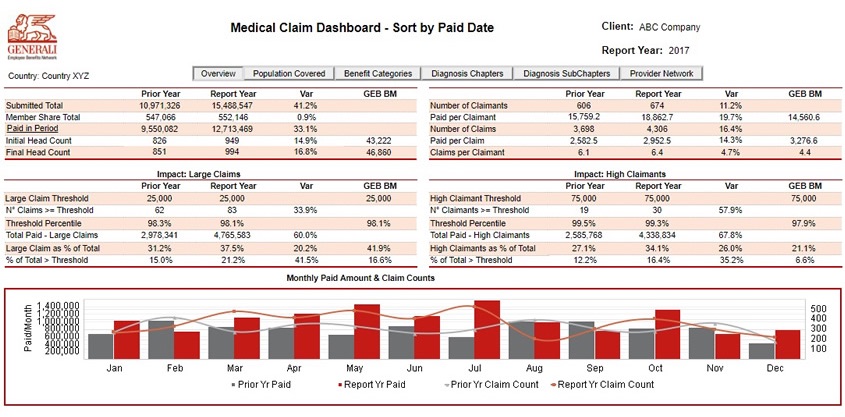
GEB pioneered global medical dashboard reports for captives in 2012, but we stepped up our game this year in terms of content, format and functionality, providing unparalleled access to clear and illuminating information.
We are now first to offer dashboard reports that are tabular (easier navigation within and between countries), interactive (drill-down capability for deeper insights) and with embedded benchmark data (immediate comparative analysis). GEB invested considerably to access more data, provide more insightful metrics, and present it all in far more usable formatting.
“We also stepped up our game in providing clients with insight,” adds Eric. “We offer individual interpretation of the graphs and tables, context about the market and local cover, and recommendations on how to mitigate trends and cost drivers.
“We differ from the market as our local focus and local knowledge makes a tangible difference, not only to costs but also in support of our key health objectives for members.”
For GEB, our mission with respect to health and wellness is to help employees and dependants:
- Stay healthy;
- Return to health, or;
- Manage chronic disease.
Data
We use data to help clients better tailor benefit plan design, wellbeing programmes, and even HR policy. Featured interactive report functionality includes:
- Detailed population data, with drilldown into related diagnostic categories;
- Detailed spending by major and minor benefit categories, with drilldown into related diagnostic categories.
- Detailed spending by major and minor diagnostic categories, with drilldown into related benefit categories;
- Detailed spending by top healthcare providers, with drilldown into related diagnostic categories.
- In all metrics, including drilldowns, the reports focus on year-over-year changes, with KPIs not just on total paid, but also on the underlying reasons for those changes, whether due to more claimants (incidence), more claims per claimant (frequency) or an increase in average cost per claim (unit cost).
Recommendations
Our reports offer clearer insights and afford more precise recommendations for clients. For example, in one instance we found an extremely high incidence of low cost, high frequency claims for colds and flus driving a client’s claim costs. We identified that local HR policy was driving these findings, as a doctor’s note was required for even one day’s absence from work, unnecessarily driving up claims for conditions where GP visits can have little impact. We recommended an HR policy change to when a doctor’s note was required, along with other initiatives to improve respiratory health overall:
- Implementation of targeted anti-cold and flu campaigns;
- An assessment of in-office air quality, and sterilisation procedures for all office surfaces;
- Implementation of an anti-smoking campaign;
- An assessment of plan design, including cost-sharing features to curb unnecessary outpatient spending;
- Implementation of a telemedicine service, to make it easier for employees to see a doctor but at a far lower unit cost.
We work closely with Network Partners to ensure plan design or wellbeing programme recommendations are feasible locally, addressing intricacies of the local environment and the interplay between public and private healthcare systems.
Supplemental support
- We help clients understand what’s already available locally (e.g remote medical second opinion, telemedicine etc).
- We identify new programmes and services to support member health and the fiscal health of global plans. In Q3 this year we rolled out to all Network Partners our new mobile health app, Ciao, designed to support behaviour change.
We are just now finishing up a new survey to Network Partners to help update our health and wellbeing capabilities grid. This information helps clients see GEB as a trusted and informed Network Provider / Partner and the information contained therein is essential for global RFPs.
“Global RFPs now ask a lot of detail about capabilities at local partner level,” explains Eric.
“They want to know whether Partners have robust
Plan Management capabilities, such as administering things like anti-fraud initiatives, flexible plan design (e.g. member co-payments and deductibles), clinical case management, prior authorisation and sophisticated claims adjudication processes.
This comes in addition to requiring detail on local capabilities around Health & Wellness, which GEB articulates into our H&W Mission structure: Stay Healthy, Return to Health and Manage Chronic Illnesses. Clients expect all of this to be communicated on a central level.
The perception is that the Global EB Network is weak if we don’t have access this information.
“We need to ensure we are a cohesive whole in order to be named as a preferred provider.”